Melanoma
The skin has four principal cell types that live on its top layer, one of which is the Melanocyte. Melanocytes are responsible for giving you your skin colour/tone and pigment. These cells respond to sun light exposure causing you to have a deeper skin tone (tan).
Occasionally some Melanocytes can take a wrong turn. They form a clone of altered cells that behave differently from normal Melanocytes and if left can replicate and divide. Once this clone of cells has reached a sufficient size it’s termed a tumour but not a cancer.
The tumour if left unchecked can grow and with time and size can invade a layer of the skin deeper to their initial superficial layer. As soon as they have passed through the barrier between superficial and deep skin layers they classify as cancer, in this case – Melanoma.
How does melanoma spread?
If left alone the melanoma can grow within the deeper structures of the skin and come across two types of vessels (blood vessels and lymph). Conventional cancers can deposit cells within blood vessels and this therefore gives the cancer a method of spreading to other areas within the body. Melanoma however is different in that it initially tends not to spread via blood vessels but prefers to spread by cells passing into lymph.
What is lymph?
Lymph is the equivalent of the bodies sewage system. Sewage leaves one’s home and passes through a series of ever increasing pipes to a sewage works where they filter the sewage through several filter beds to purify and clean, leaving potential clean “water”.
The body likewise produces waste products from all its cells which along with viruses and bacteria should avoid the blood circulation due to their toxic effects. The body therefore passes these waste products through a series of lymph vessels to filter beds (lymph nodes).
These nodes are found throughout the body but conventionally we think of them lying in the groin, arm pit and neck. These nodes respectively filter the lymph from the leg, arm and head and neck.
Areas such as the torso and chest can pass to one or many of these sites. Lymph drains from all these sites centrally and at certain intervals following lymph node filtering they deposit the “clean lymph” into the blood.
How serious or not so serious is my Melanoma?
We grade how serious one’s Melanoma is by a staging system. This is a complex and potentially confusing system but the general message is that the longer one has had melanoma the higher the likely hood that the Melanoma has grown and or spread.
The depth of the melanoma measured in mm gives an indication of melanoma progression within the skin and the potential likely hood that it could have invaded vessels such as lymph vessels. Knowing whether the melanoma has spread to the lymph node however gives us a key indicator of one’s Melanoma status.
If Melanoma initially principally spreads to the lymph nodes first then if the lymph nodes are clear then it is highly likely that the melanoma progress is still on the skin. If however the lymph nodes harbour Melanoma then this may be concerning news.
Nevertheless to know that it has spread is beneficial in that this allows patients to begin therapies such as Immunotherapy as soon as possible that could prevent further spread or melanoma progression.
The process by which surgeons sample the first lymph node that the Melanoma would spread to is Sentinel Lymph Node Biopsy (SLNB).
How do we locate the first lymph node that the Melanoma could drain to (the Sentinel Node)?
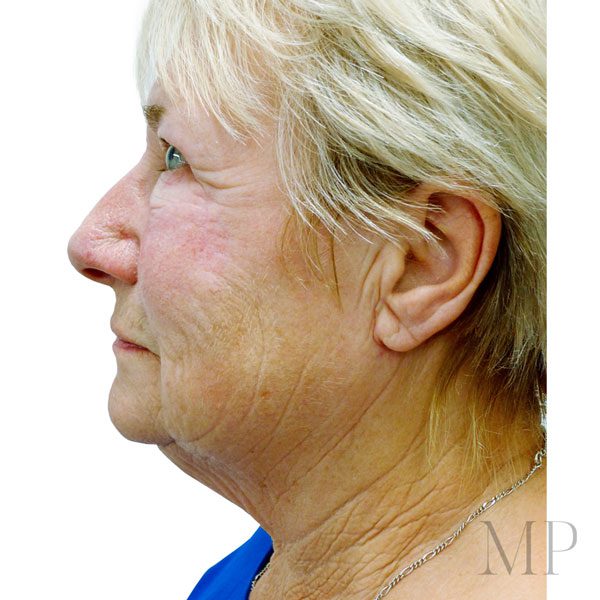
Most melanomas referrals to us have had an excision by taking a minimal margin of skin around the lesion. This is mostly closed directly leaving a linear scar.
The centre of the scar is therefore as close to the epicentre of where the melanoma once was. This central aspect of the scar should have the same draining lymph channels and the same Sentinel Node.
Injecting the centre of the scar with a radio-opaque tracer that passes to the Sentinel node will show the site of the sentinel node on a specialist X-ray. Injecting the same site with a coloured dye will also mean that we will stain the sentinel node the colour of the dye helping differentiate this from other non Sentinel nodes.
This is conventionally done under a General anaesthetic of 2 hours duration if the Melanoma was within the Head and Neck. We inject the radio-opaque dye either the day before or the morning of the procedure.
Once the x ray has been taken the radiographer will mark on the skin the site of the node, cross referencing to the radiographs. Mr Potter will review both the skin marks and the radiographs. Once under general anaesthetic we will inject your scar with a bright blue dye (the second SLNB tracer) and the melanoma scar will be excised with a suitable margin to minimise the chance of the Melanoma recurring within the skin.
The defect post skin excision is commonly closed directly or with the assistance of local flaps of skin or skin grafts, using skin from the local area to give an even skin colour match.
We remove the sentinel node often through a separate incision in a pre-existing skin fold within the neck. Occasionally, we remove two nodes, but this is rare. Once the node has been removed we close the neck, commonly with dissolving sutures.
Post Operative
Post operatively we will encourage you to get all operative sites wet under a shower the day after and every subsequent day, with soap and water. Mr Potter rarely uses dressings within the head and neck for ease of wound care. A week after the operation, you are to attend for a wound check if needed and reviewed as soon as the node biopsy result has returned. This commonly takes two weeks.
Finding the draining Sentinel Node is thought to be more challenging within the head and neck than other sites. This principally is due to the fact that the neck has more nodes per side than the groin or arm pit. The neck is also the highway for nerves leaving the brain and for vessels supplying blood to the brain. For this reason sentinel lymph node biopsy of the head and neck is only undertaken within a few centres in the UK and world wide.
As there are generally over 100 nodes within each side of the neck the chance of sampling the wrong node and leaving the sentinel node is potentially higher than at other sites. Thus if this node were to be negative then there is the chance of leaving behind a positive node. We call this phenomenon “the false negative”.
The lower a surgeons false positive figure the lower the chance of incorrectly sampling the node and the higher the chance of obtaining the sentinel node. Thus surgeons aim for a very low false negative figure.
The medical literature has reviewed the false negative rates of head and neck sentinel node sampling in melanoma and figures vary from 4-8%. Matthew has reviewed his sentinel node false positive rate. He has a rate of 0% and therefore has not taken out the incorrect node to date.
Matthew Potter’s SNLB Experience
Matthew has been undertaking sentinel lymph node biopsies for melanoma of the head and neck since 2011. He has been undertaking sentinel node biopsies at non head and neck sites since 2005 and has published his series of head and neck SLNBs of over 150 patients. This is the largest published series within the UK, we believe this to be the second largest solo surgeon series world wide. No other published series world wide has a false negative rate equalling 0%.
Matthew is a Macmillan Adopted Consultant and works within a team of Melanoma specialists in Oxford and Swindon. This team includes
1. Macmillan Nurse Key Workers
2. Professor of Melanoma Medicine
3. Melanoma Radiation Oncologists
4. Melanoma Immunotherapy Oncologists
5. Dermatologists with a specialist interest in Melanoma
6. Radiologists with a specialist interest in skin tumours and the early detection of distant disease spread
The Sentinel node shows whether your melanoma has spread or not. This gives us information with regards to survival. One of the largest international studies of Melanoma has shown that if your melanoma is of intermediate thickness, those that have a negative sentinel node have an 80% chance of being alive at 10 years.
If you have a positive node from Sentinel lymph node biopsy then the chance of you being alive at 10 years is 60%. If you don’t have a sentinel lymph node biopsy but go on to develop a spread of melanoma to the nodes the chance of being alive at 10 years is 40%.
A positive sentinel node this means that you will see a medical oncologist and will undergo regular surveillance scanning for blood born spread of the disease. By having regular scans and detecting a blood born spread early means that we could place you on Immunotherapy earlier.
We believe that by this aggressive investigation protocol our patients get to immunotherapy as soon as possibly giving them the best chance for them and their melanoma.
Matthew’s data shows that of those with a positive sentinel lymph node the chance of then progressing to having spread in the blood stream is 30%. If you have a negative lymph node the chance of progressing to blood born spread is 7%.
From Matthew’s patient outcome data we have shown that the chance of dying from melanoma if you have a positive sentinel lymph node is 7%. If your node is negative the chance of dying from Melanoma is 2%.
It shows that the Melanoma has spread to the lymphatic system. Patients find this news alarming and sometimes devastating. Whilst this is disappointing it is advantageous that we are aware that it has spread. Detecting the spread through Sentinel node biopsy means that this has detected spread at a microscopic level.
We hope therefore that the Melanoma confines to the lymphoid system. The goal at this stage is to make sure that there is no evidence that the melanoma has spread into the blood and we evaluate this by a CT scan.
We will review this scan in Oxford by a Consultant Radiologist with a specialist interest in Melanoma and the scan and your situation discussed at the Skin Multi Disciplinary Team (Skin MDT) meeting in Oxford.
If the scan is clear then we will offer you a completion neck dissection. This procedure takes the majority of a day to perform and removes all the nodes on the side of the head and neck on the side of the previous sentinel node. The aim of this procedure is to ascertain any other involving nodes and to get ahead of the lymphatic spread.
Matthew has undertaken over 150 neck dissections. His return to theatre rate and complication rate for this procedure is less than 1%. Following the neck dissection your pathology will be further reviewed at the Skin MDT and at this stage where appropriate you could be offered Immunotherapy or Radiotherapy. The need for radiotherapy or immunotherapy after neck dissection is rare. Patients at this stage go on to having regular surveillance scans and reviews.
Mr Potter has not had a single patient relapse within the neck following sentinel lymph node biopsy. This applies to those with either a negative or positive node. Despite this we will review your neck every three months along with a top to toe skin check.
This review applies for the first three years of follow up. From then on we will review every 6 months. Where applicable we share this review with referring clinicians nearer you, Oxford Oncologists or a unit closer to you.
Recommended Websites:
1. http://genomel.org/news/option-grids-information-for-melanoma-patients/
2. http://www.melanomauk.org.uk/
3. http://www.skcin.org/
4. https://www.macmillan.org.uk/information-and-support/melanoma
5. https://melanomafocus.com and melanoma focus helpline www.melanomafocus.com/support/ helpline
Melanoma Support Group Information
- Melanoma Mates – a closed group (face book group) for patients and families offering friendship, support, shared experiences and information.
- http://www.melanomarollercoaster.co.uk/25-new-year-new-me/
- Melanoma UK digital registry melanomauk.org.uk/registry
- www.melanomafocus.com/support/helpline
Melanoma & Diet | Helpful Websites:
- https://www.cancer.gov/about-cancer/treatment/side-effects/appetite-loss/nutrition-pdq/
- www.guysandstthomas.nhs.uk/resources/patient-information/cancer/diet-and-
chemotherapy.pdf

Matthew’s Melanoma data
Total number of Sentinel nodes undertaken within the head and neck
Greater than 250
Percentage of removing the correct lymph nodes
99.7%
Percentage with Positive nodes
15%
Percentage return to theatre following Sentinel node biopsy
1%
Percentage nerve injury following SLNB
0%
Percentage with local recurrence following wide excision of the melanoma
0%
Percentage of SLNB cases that were aborted
1%
Percentage of cases - day cases
82%
Percentage of cases not discharged after one night
1%
Distribution of age of patient
21-96
Percentage of cases undertaken over 80 (and number)
20%
Percentage of complications in those under 80
The only two return to theatres cases were under 80
Percentage return to theatre following neck dissection
Less than 0.3%
Percentage of nerve injury/complication following neck dissection
nil
Percentage rate of other nodes involved within the neck dissection specimen
8%
Percentage survival of those with a negative SLNB
98%
Percentage survival of those with a positive node
93%
Percentage relapse of Melanoma within the head and neck following Wide Local Excision and Sentinel Lymph Node Biopsy.
0%
Matthew will discuss all the risks associated with the procedure in detail with you in clinic to allow you to make an informed decision as to whether you feel a Sentinel Node Biopsy is appropriate for you. Like the list of side effects on all medication leaflets, the list of operative risks has to be lengthy as any potential risk should be discussed. In short the only complication Matthew has had following this procedure is a return to theatre the following day due to a small bleed under the skin. This has occurred in two patients. in both cases the patient had a return to theatre and was discharged a day later than planned.